What is missing from mainstream psychology?
Structural/social inequality
Political or social consciousness emerged in my early teens through a combination of Jon Stewart’s ‘The Daily Show’ and reading the Autobiography of Malcolm X. I often try to empower the youth I work with on the importance of understanding history, politics, economics and social change.
I have been a part of MAPS (multidisciplinary association for psychedelic studies) for over 5 years; more than drug reform, the organization seeks to shift our societal understandings away from ‘drugs’ as recreational or pleasure-seeking towards healing (within safe clinical boundaries) – to learn more, click here
Scene from Avengers Endgame (2019) showing a depiction of group therapy for individuals suffering from the death of a loved one.
Many places of worship also offer support groups (or ought to if they do not) and it is recommended for those whose beliefs align with any religion, to bridge any individual growth with communal wholeness. It is a saying from our Holy Prophet, ‘the believers are reflections of one another’ and so let us always seek to find a tribe that nurtures our psyche and spirit.
Although the focus of this website (and my career broadly speaking, as well as many others) is a re-integration of spiritual ideals, rituals and principles to account for a more holistic narrative of the human experience, even that may ‘miss the boat’ (for more information, you can visit the ‘Dark Side of Spirituality‘ tab).
A recent APA survey found that financial inequality is the most common source of stress for Americans. How much cognitive reframing can someone do if they fear crippling financial debt and homelessness? Should we tell these people to just ‘take a few deep breaths’ and let the calm wash over them? Or is there a certain responsibility we each have to care for and create equitable systems built on reciprocity and accountability?
I am not discounting the role of individual change; even through the most decrepit suffering, a person with a solid character has more robust opportunity, know-how, resources and sources of support to help them (whereas a faulty person has nowhere to turn, who will trust them when they have burnt all their bridges?).
What more can be done?
- Interdisciplinary approach to treatment; I have been struck time and time again by the needless red-tape and administrative nightmare in ‘reaching across’ for coordinated help with a youth. For example, when I worked at a school district and needed help with a child, it took months on end to hear back from the primary physician or psychiatrist. I believe this can be traced to graduate school and how education is broadly taught. Each discipline of health is subsumed under the weight of their own theories and practice, with little consideration for the importance of working together.
- Lobbying for local and national-level policy; I can give my own small example here. School districts have a zero-tolerance policy for drugs, hence there are countless youth who are needlessly suspended or expelled and forced to undergo psychological testing for such a minor issue like a vape pen being found in their backpack. In the worst of cases, they are even sentenced to jail which drastically increases their chances of dropping-out early and subsequent issues as adults. Whatever political ideology one supports, mental health professionals must strive towards common sense law reform.
- Communal integration; ‘the child who is not integrated into the village will burn it down just to feel its warmth.‘ We cannot be alone, even the most solitary person risks drastic health impairments without ones to provide solace and support. Individual treatment should always be supplemented with group or communal integration. For example, NAMI (National Association of Mental Illness) offers free support groups across the U.S. for family members and individuals.
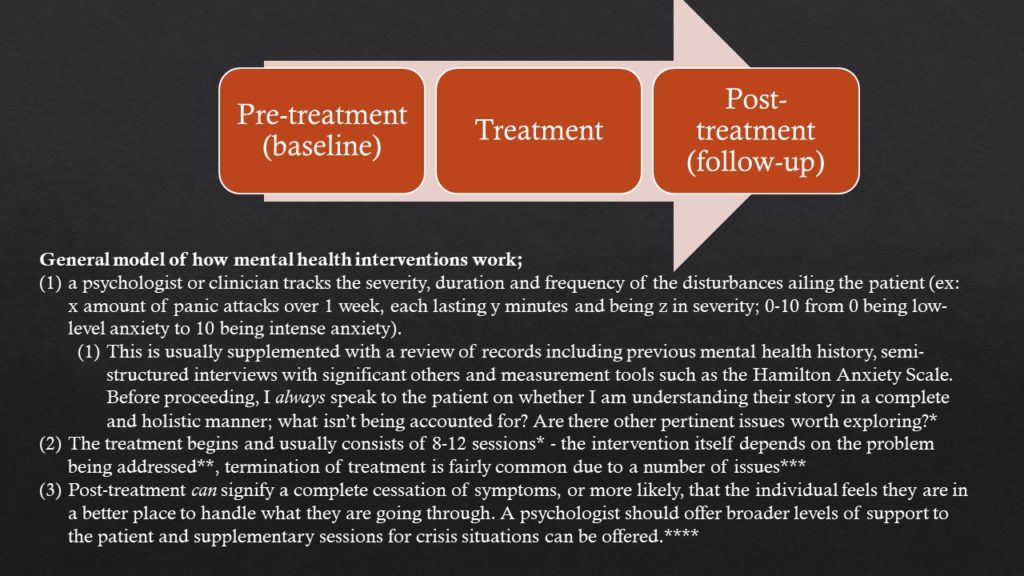
* Most health insurance policies indicate 8-12 sessions for diagnosable mental health illnesses.
** Intervention can be adapted and modified depending on presenting issue and setting (i.e., each clinic may specialize in certain illness such as substance abuse, family, marriage, etc. and a person may be referred elsewhere if the clinic does not match patient’s profile).
*** Many treatment sessions (around 30-40%) end after the first or second session due to poor rapport between client and patient, lack of accessibility such as patient not being able to take time from work or family, inadequate treatment fit, etc.
**** For example; many mental health professionals offer group therapy for individuals; hence, a person can benefit from one-on-one treatment and finding others who are going through similar issues for broader effectiveness.
